A Welcome from the Program Director
The Kirk Kerkorian School of Medicine at UNLV emergency medicine residency was developed from the ground up by a dedicated faculty, hailing from both community and academic backgrounds, with a shared common vision of a model program — one which would embody the next generation of emergency medical education. Preparation to confidently manage ‘any patient in any situation’ is the bare minimum that should be expected from a residency program, as success in the ‘real world’ after residency is predicated on a multitude of factors beyond raw medical knowledge and procedural skills.
Present-day emergency departments demand physicians with a mastery of departmental patient flow, clinical productivity, documentation, patient satisfaction, communication skills, team leadership, and the delivery of safe, high-quality patient care. Purely academic residency programs may fail to provide adequate preparation in one or more of these essential skills, while community programs may lack the academic rigor or diversity of population that many seek. The design of our residency program combines the academic and operational training necessary to flourish in the complex environment of today’s emergency departments, with the stimulating hands-on clinical experience found in the setting of a high-acuity county facility.
The clinical and didactic curricula of a residency program should not be static – instead, the leadership of our residency recognizes that the ability to provide the highest quality care on the front lines of medicine requires training that remains ahead of the curve. Our residency program encourages and responds to the feedback from its residents, takes the time for self-reflection, and strives to continually evolve by refining our curricula. We set the bar high for ourselves, as do our residents, on our path to becoming one of the premiere programs in the country.
I encourage you to explore our website to gain some insight into the residency experience and sense of camaraderie offered at our program. Life should not be put on ‘pause’ during residency – come share the next phase of your medical training with a dynamic group of colleagues who epitomize the concept of leading balanced lives while remaining engaged in education and community involvement, and embarking on a path to leadership.
— Ross P. Berkeley, MD, FACEP, FAAEM
Residency Program Director
Vice Chair for Quality & Education
Contact
901 Rancho Lane, Ste 135
Las Vegas, NV 89106
Please contact us about questions you may have regarding your application to the program and interview.
Phone: 702-383-7885
Fax: 702-366-8545
About the Program
The Kirk Kerkorian School of Medicine at UNLV emergency medicine residency was developed from the ground up by a dedicated faculty, hailing from community and academic backgrounds, with a shared vision of a model program - one which would embody the next generation of emergency medical education. Preparation to confidently manage ‘any patient in any situation’ is the bare minimum that should be expected from a residency program, as success in the ‘real world’ after residency is predicated on a multitude of factors beyond raw medical knowledge and procedural skills. Present-day emergency departments demand physicians with a mastery of departmental patient flow, clinical productivity, documentation, patient satisfaction, communication skills, team leadership, and the delivery of safe, high-quality patient care. Purely academic residency programs may fail to provide adequate preparation in one or more of these essential skills, while community programs may lack the academic rigor or diversity of population that many seek. The design of our residency program combines the academic and operational training necessary to flourish in the complex environment of today’s emergency departments, with the stimulating hands-on clinical experience found in the setting of a high-acuity county facility.
The clinical and didactic curricula of a residency program should not be static – instead, the leadership of our residency recognizes that the ability to provide the highest quality care on the front lines of medicine requires training that remains ahead of the curve. Our residency program encourages and responds to the feedback from its residents, takes the time for self-reflection, and strives to continually evolve by refining our curricula. We set the bar high for ourselves, as do our residents, on our path to becoming one of the premiere programs in the country.
Curriculum
We are proud of the residency training we provide and continually strive to improve the education we offer. Resident feedback is taken seriously by the program leadership and has been integral in refining our didactic and clinical curriculae in order to ensure that our training program stays ahead of the curve. The clinical environment in which we work provides an incredible hands-on experience for residents, with an unparalleled variety and severity of pathology, and is augmented by our innovative didactic education.
We are one of the few three-year residencies to offer a four-week elective rotation during the PGY-2 year, in addition to a second elective in the PGY-3 year, to allow residents an opportunity to gain exposure to areas of interest earlier in their training, so they can make a more informed decision regarding potential fellowship choices.
Take some time to explore both aspects of the curriculae below:
PGY-1
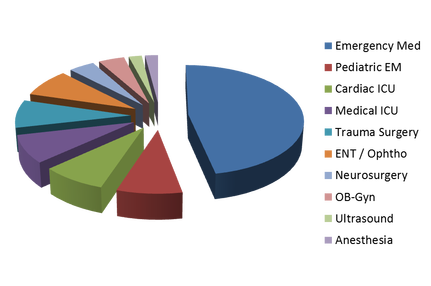
Your first year in Vegas throws you right into the action. Our first-year residents are afforded the opportunity to evaluate patients of any acuity level, including the critically ill, and spend 21 weeks in the emergency department. Other areas of focus include four weeks of trauma surgery (spent at the only Level I Trauma Center in the state), as well as eight weeks on critical care services. The year also includes two weeks each of ENT, neurosurgery and obstetrics and gynecology, as well as 1 week of anesthesia and 1 week of ED ultrasound. Our PGY-1 residents receive a very well-rounded experience, and many complete the year having logged enough procedures to fulfill residency graduation requirements.
PGY-2
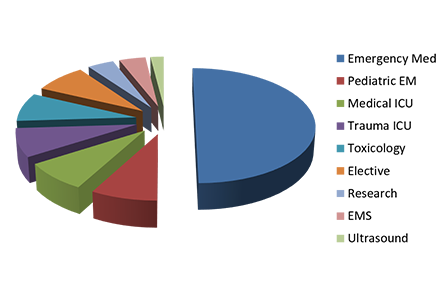
The second year in Vegas sees more emphasis placed on emergency medicine, with 25 weeks spent in the emergency department. Our curriculum stays ahead of the curve with eight more weeks of critical care training. The trauma ICU, which is consistently rated as one of the best rotations, permits significant resident autonomy and affords a high number of procedures. PGY-2s also get to travel to Denver for four weeks to rotate at the Rocky Mountain Poison & Drug Center, one of the premier toxicology sites in the nation. It is in the second year that our residents really hit their stride as emergency physicians.
PGY-3
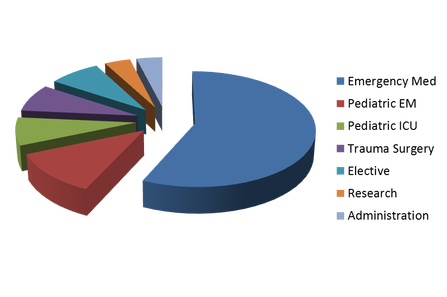
Our senior residents are amongst the best in the country. By the end of training, our residents are capable of landing fellowships, academic positions, or highly competitive jobs in a community setting. The final year of training truly sets all Vegas residents up for this success. The majority of the year is spent in the ED (33 weeks total) with an additional four weeks of trauma surgery and four weeks of pediatric ICU - continuing the emphasis on critical care. While in the ED, senior residents run the department, focusing on teaching junior residents and rotating medical students.
Emergency Medicine, Grand Rounds
Emergency Medicine Grand Rounds are held weekly on Wednesday mornings in our departmental conference room, which was recently expanded and outfitted with an updated AV system. Faculty, residents, and departmental staff are invited, and this is protected time (no clinical duties) for the emergency medicine residents. Our conference is constantly evolving in order to remain at the cutting-edge of education and provide the highest-yield learning for our residents. This time is fun and collaborative, and often leads to lively discussions. Regular features include:
- ACES: boards-style quizzes and review
- Case Conference Series
- Core Content Lectures
- Radiology Rounds
- EKG Rounds
- Morbidity and Mortality Conference
- Ultrasound Lectures and Skills Labs
- Research Methodologies Series
- Guest Lectures via Videoconference
Mock Oral Boards
One of the many goals of residency training in emergency medicine is preparation for passage of the ABEM (American Board of Emergency Medicine) certification examinations. To this end, our residents participate in Mock Oral Boards once per quarter during Wednesday Grand Rounds. Under the direction of Dr. Berkeley, the cases are designed to challenge the residents, as well as develop consistent and effective test-taking habits via regular practice. Many of the emergency medicine faculty, including Drs. Baydoun, Berkeley, Cleveland and Young, serve as instructors at the national AAEM Oral Boards Review Course.
It is our expectation that all graduating residents will be fully prepared to take the ABEM Oral Boards Examination and will feel confident in their test-taking abilities.
Simulation Lab
The Nevada System of Higher Education recently opened a multi-disciplinary, multi-institution Simulation Center clinical skills laboratory, which is used on a regular basis by the Emergency Medicine residency. Simulation days occur quarterly and are usually in conjunction with emergency ultrasound skills labs. Jordana Haber, MD, our simulation director, has developed a comprehensive battery of challenging and engaging scenarios. This is not about the adoption of technology for its own sake, but rather the enhancement of training by providing an opportunity for residents to develop resuscitation leadership skills and master the management of high-risk ED scenarios.
The 31,000 square-foot facility houses a fully integrated space for high fidelity simulation, standardized patient instruction, and procedural skills development. There are separate debriefing rooms that also allow remote viewing of simulations in action, classrooms for instruction sessions, as well as a lecture hall. The simulation facility is also used by other residents and medical students from the University of Nevada School of Medicine, as well as nursing students from the University of Nevada Las Vegas and Nevada State College.
Journal Club
Held on the fourth Tuesday of each month at the home of one of our faculty or at a local park, Emergency Medicine (EM) Journal Club provides an opportunity for faculty, residents, and students to get together in a relaxed and informal environment to discuss pertinent EM literature and topics. Journal Club is led by David Slattery, MD, the departmental research director, and helps residents put into practice the critical appraisal skills taught in the research lecture series. Lively debate regarding evidence-based medicine is the norm, as the group critically reviews the recent scientific literature in order to determine its applicability to clinical practice in the ED.
Training Sites
The Kirk Kerkorian School of Medicine at UNLV utilizes the University Medical Center (UMC) of Southern Nevada, the premier academic and tertiary care hospital in the state, as its major teaching hospital. With the only Level I Trauma Center in Nevada, UMC also offers extensive specialist coverage, including pulmonary and surgical critical care, HIV-medicine, gastroenterology, nephrology and transplant nephrology, hematology/oncology, cardiology, neurology, interventional radiology, general surgery, pediatric surgery, trauma surgery, ophthalmology, otolaryngology, urology, obstetrics and gynecology, pediatrics, and, psychiatry. Last year, UMC provided outstanding emergency care and service to over 125,000 patients, including 33,000 pediatric and 11,000 trauma patients.
Emergency Medicine Department Initiatives at UMC
First developed in 2006 by Dr. Ross Berkeley, Kirk Kerkorian School of Medicine at UNLV professor, and Vice Chair for the Department of Emergency Medicine, the UMC Cardiac Activation system facilitates rapid patient stabilization and transfer to the Cardiac Catheterization Lab for emergent percutaneous coronary intervention (PCI), available 24 hours a day, seven days a week. Dr. Berkeley continues to coordinate the UMC Cardiac Activation system for emergency department management of patients with acute ST-segment elevation myocardial infarction (STEMI). Under this program, the door-to-balloon (D2B) time for emergent PCI has dramatically improved, with consistent achievement of D2B times <90 minutes. UMC is a Joint Commission certified Acute Myocardial Infarction (AMI) Center with the American College of Cardiology - Platinum Achievement Award for AMI.
PGY-3 emergency medicine residents are able to initiate the Cardiac Activation system, which activates the Catheterization Lab, once they demonstrate clinical competency in EKG assessment.
The UMC stroke management program began in part as a PGY-3 emergency medicine resident healthcare delivery project, and has evolved into a fully-developed system throughout the institution, which is certified as a Primary Stroke Center. A 'Code White' activation is initiated for patients who present with signs of acute stroke, which facilitates rapid mobilization and coordination of hospital resources, including stat CT availability and involvement of a stroke neurologist. UMC is a Joint Commission certified Primary Stroke Center with a Gold Plus Achievement Award for Stroke.
Kirk Kerkorian School of Medicine at UNLV Associate Professor Dr. David Slattery developed the Las Vegas program to initiate pre-hospital hypothermia on patients with return of pulses after cardiac arrest. He spearheaded the implementation of the UMC therapeutic hypothermia program, with the goal of improving neurologic outcome in patients who remain unconscious after successful resuscitation from cardiac arrest.
Developed in conjunction with a multi-disciplinary team, a standardized protocol is utilized to help identify and rapidly resuscitate patients with severe sepsis and septic shock. Elements of early goal-directed therapy, both invasive and non-invasive, are applied to improve patient outcome.
Always ahead of the curve, the UMC Adult Emergency Department has had a physician-in-triage program since 2009. Medical director Dr. J.D. McCourt and assistant medical director Dr. David Obert redesigned the triage process in 2011, with the goal of having patients evaluated by a physician as soon as possible after arrival. Termed Rapid Medical Assessment (RMA), this streamlined process provides improved patient care and safety while addressing critical issues of ED wait time and overcrowding. The key to success is surrounding the patient with a triage team with the authority and tools to make a rapid assessment, initiate care orders and determine the next steps in evaluation and management— before patients are even brought back to an ED room. The RMA process has greatly improved the door-to-doctor time for patients presenting to the Adult ED.
Kirk Kerkorian School of Medicine at UNLV Professor Dr. Ross Berkeley, director of the UMC Chest Pain Center, has worked collaboratively with members of the Emergency Department, Cardiology Department, and Internal Medicine to refine and streamline the protocol for assessment of patients experiencing acute chest pain. After initial evaluation and management in the Emergency Department, patients at low to intermediate risk of acute coronary syndrome are admitted to a discrete unit staffed by specialized RNs. The Chest Pain Center's systematic approach to patient evaluation and accelerated diagnostic protocol allows for thorough, yet cost-effective and rapid assessment.
UMC’s Chest Pain Center, the first full-scale chest pain evaluation center in Nevada, was established in 1996. UMC achieved status as an Accredited Chest Pain Center with PCI by the Society of Cardiovascular Patient Care in 2009.
How to Apply
We participate in the Electronic Residency Application Service (ERAS). Hard copy applications cannot be considered. We currently have no unexpected vacancies in the residency and all of our applicant positions are committed through ERAS and the National Residency Match Program (NRMP) only.
All correspondence regarding the status of your application is conducted by email. Therefore, applicants should have a reliable email address that is checked in a timely manner. If you have additional questions, please call 702-383-7885, or send us an email at emergencymedicine.residency@medicine.unlv.edu.
- September 1 - Applicants may begin selecting and applying to residencies
- October 1 - Medical Student Performance Evaluations (MSPEs) are released
- November 7 - Deadline for completed applications to be received by our program
- Mid-November through Late January - Interviews conducted. See Interview Day Details below for more information.
- February - Deadline for finalizing rank lists for both applicants and residency programs
- ERAS Common Application
- Medical Student Performance Evaluation (MSPE) - [medical school dean’s letter]
- Three letters of recommendation (two of which must be written by emergency medicine physicians). Those provided by emergency medicine specialists must use the Council of Residency Directors (CORD) Standardized Letter of Evaluation (SLOE) template, formerly called the SLOR, which can be downloaded from the CORD website.
- Step 1 United States Medical Licensing Examination (UMSLE) or Step 1 National Board
of Osteopathic Medical Examiners (NBOME) transcripts - Medical school transcript
- Personal statement
The United States Air Force, the Kirk Kerkorian School of Medicine at UNLV, and the University Medical Center of Southern Nevada (UMC) — have joined forces to produce an exceptional emergency medicine residency program for active duty Air Force personnel. Keep this in mind as you apply for a residency: UMC, where you will do the vast majority of your clinical education training as well as didactics, has Nevada’s only Level I Trauma Center as well as the state’s only Burn Center — the surgical teams there are so remarkable that the National Trauma Data Bank has found that of those who arrive alive (many have less than a 1 percent chance to live) more than 96 percent survive and are discharged.
Emergency medicine is a very competitive field for all applicants and particularly so for those on active duty in the Air Force. Of the 10 residencies offered through the Kirk Kerkorian School of Medicine at UNLV and UMC. two are designated for Air Force personnel. It is strongly encouraged that you complete a clinical rotation at our program for consideration during the Joint Services Graduate Medical Education Selection Board (JSGMESB, also known as the military match). During this program, residents are “stationed” at Nellis Air Force Base and do three months of clinical rotations at the medical there, but complete nearly three years of their requirements at UMC. Active duty residents enjoy higher pay than their civilian counterparts as well as Tricare insurance for themselves and their families.
Interviews will be granted after review of a completed application. Candidates will be contacted via email by the program coordinator if granted an interview. Interviews occur on Wednesdays at our administrative office located at 901 Rancho Lane, Suite 135 (corner of Rancho Lane and Tonopah Drive). As a result of the format, candidates are able to attend our weekly Grand Rounds conference series when they are not interviewing with one of the faculty or Chief Residents, as well as spend additional time interacting with the EM residents during lunch.
During the interview season, you will have a dedicated resident liaison who will contact you via email the week before your interview day, to help guide you through the process. Candidates are strongly encouraged to attend the resident 'Meet & Greet' dinner that takes place on the Tuesday evening prior to the interview day, which provides an opportunity to get to know our residents in an informal setting and gain an appreciation of the sense of camaraderie here. Candidates are also invited and encouraged to do a 'shadowing shift' within the University Medical Center (UMC) Emergency Department, either before or after the interview day, in order to develop additional insight into the dynamic setting of our program.
Candidates have previously had success staying at the SLS Hotel, which tends to have reasonable rates and is less than 2 miles from your interview location.